By Daniel K. Brantley
For appropriate adolescent patients, bariatric surgery overcomes genetic propensity to obesity, though the exact mechanism is yet unknown.
Charts and percentiles determine weight goals within the adolescent population. Those young patients whose weight goes beyond the ideal traditionally have a single prescription: a healthy lifestyle, including diet and exercise. Unfortunately, this is not always successful. The result? Feelings of guilt and inadequacy in both parent and child, which does not aid in weight loss.

According to Hesham Atwa, MD, FACS, FASMBS, a new approach is required. His perspective is based on recent research that indicates providers should not rely solely on lifestyle modification when genetics may be the root cause of obesity. Rather, they should tell young patients something they’ve never heard: It’s not your fault.
“When they come to me, I ask why they think they’re overweight, and 90% say because they eat too much or don’t exercise,” Dr. Atwa says. When he explains that obesity is not the adolescent or teen’s fault, many get emotional. It is the first time they’ve heard such a statement, and the impact is profound. “[The medical community] never points a finger for having … cancer,” says Dr. Atwa. “Obesity is a medical problem.”
The AMA confirmed the designation of obesity as a disease in June 2013. Despite this, much of the medical community continues to consider childhood obesity a personal choice that can be overcome with a commitment to lifestyle changes. Dr. Atwa, Founder and Clinical Director of Long Island Laparoscopic Doctors, says this approach fails children and sets them up for a lifetime of obesity that cannot be overcome without medical treatment.
The Preferred Option
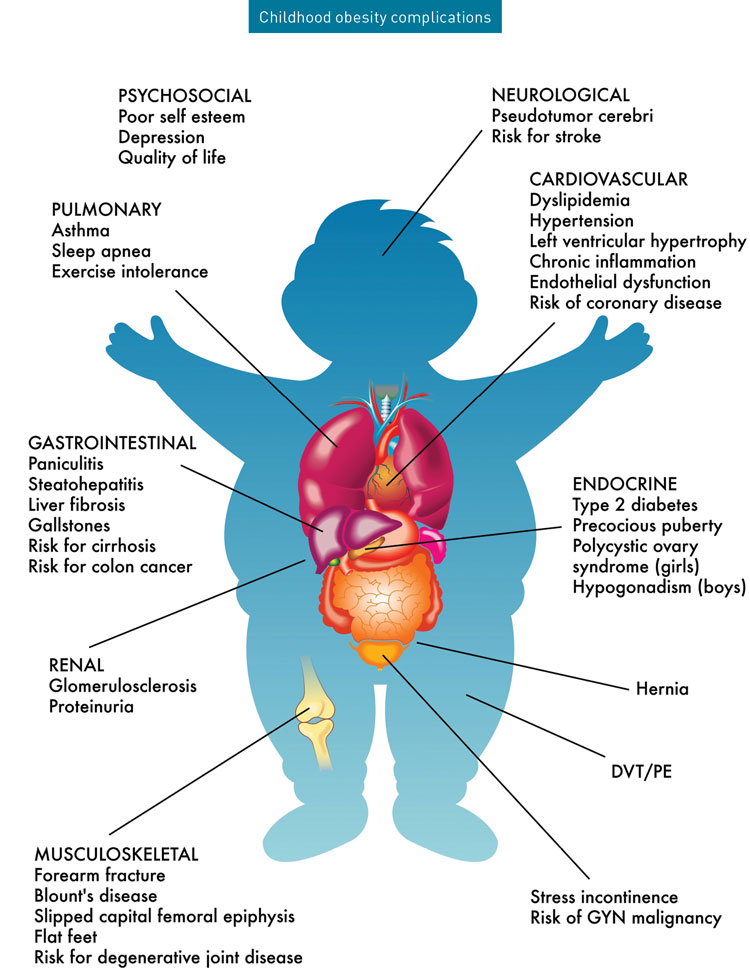
Today, nearly 20% — more than 14 million — of American children and adolescents are obese. One study showed that quality of life scores for obese children and adolescents are equivalent to those of children diagnosed with childhood cancer. However, the complications of childhood and adolescent obesity do not end with childhood. Left untreated, obese children and teens have a nearly five-fold risk of adult obesity, and 70% of them will continue in obesity after age 30.
Once in adulthood, they have access to multiple treatment approaches. Diet and exercise, medication and bariatric surgery all offer positive results when applied appropriately. Beneficial as these therapies are, waiting to treat the disease comes with a myriad of risks. Minimizing or avoiding these risks requires that obesity be treated as early as possible. Among adolescents and teens, Dr. Atwa has found that the most effective treatment option for long-term weight loss is bariatric surgery.
This finding is likely due to the nature of obesity during the early years. Adolescent obesity seems to have a genetic proponent that functions alongside environmental, personal and medical factors. The respective three- to ten-fold increased obesity risk if one or both parents are obese demonstrates this genetic connection.
Affected children have a genetic predisposition to increased hunger, but they do not eat uncontrollably, as some imagine. Even with this genetic caloric craving, on average, Dr. Atwa states that obese children consume only 100 calories more each day than their non-obese counterparts. And the latest findings reveal that the genetic predisposition to childhood obesity is not solely caused by the parents. Instead, such a predisposition takes root two generations prior.
“People say that genes don’t just change in four generations, and that’s not true,” Dr. Atwa says. “Actual genetics change over thousands of years, but we’re talking epigenetics, and these [changes occur] within a generation or two.”
The source of these changes resides within the obese child’s grandmother. While in utero, the grandmother is exposed to a toxin. This impacts the grandmother’s genetics in such a way that the grandchild is at increased risk of experiencing obesity or morbid obesity.
Though there is some question about what introduced toxin could cause this dilemma, Dr. Atwa suspects responsibility lies with the variety of changes that occurred within food and drink over the last sixty years. Diet soda, low-fat foods, chemicals, preservatives and improved agricultural genetics that allow for the production of more food quicker may all contribute. A departure from ancient grains may also play a role. When seeking a healthy choice, many opt for whole-grain bread. Though a better option than white bread, Dr. Atwa states that whole-wheat bread causes a higher glucose spike than a candy bar.
Risks of Unchecked Obesity
Children, adolescents and teens face many of the same risks from obesity as adults. For example, their lifetime risk increases for dangerous and deadly conditions such as heart disease and diabetes, high blood pressure and cholesterol, kidney problems, fatty liver, and sleep apnea. Many of these risks do not have immediate effect. Rather, they are complications that arise from years of obesity. Obesity in childhood jumpstarts the process toward such disease.
Regardless of how long the issues take to manifest in physical symptoms, they result in lower quality and quantity of life.
“[For the] first time in our lifetime, children are going to live shorter [lives] than their parents because they’re so overweight,” Dr. Atwa says. “All these medical problems are accelerated in kids. The earlier you catch the problem, the more likely you can resolve it.”
Managing Risks through Surgery
The resolution offered through adolescent bariatric surgery is significant. On average, adolescent bariatric surgery patients lose one-third of their excess weight within the first 9–12 months. This comes with the benefit of resolving comorbidities brought on by obesity.
Following bariatric surgery, resolution rates among adolescents and teens are:
- Hypertension — 100% resolution
- Diabetes — 94% resolution
- Sleep apnea — 91% resolution
This bodes well for the long-term health of patients, as adolescent bariatric surgery protects the heart, brain, joints, and other organs and body systems throughout life.
Other benefits are more difficult to measure statistically, but they are just as instrumental to a young person’s health and well-being. During the teenage years, obese individuals may experience bullying, which the current digital environment only amplifies. Obese adolescents and teens may struggle with self-esteem. They’re more likely to sleep poorly and to lack focus and sufficient energy for activities of daily living. Body image, energy levels, personality and ability to focus and perform schoolwork or function within the workplace are all affected by obesity.
“There are many medical [issues] caused by being overweight,” Dr. Atwa says. “Yet you don’t go to the hospital because you’re obese. We treat some of the medical problems, but it’s essential to treat the cause of all these medical issues.”
Resolving the underlying disease — obesity — improves all these areas. Ultimately, early bariatric surgery increases quality-of-life scores for appropriate adolescents and teens.

Timing the Procedure
Currently, the American Academy of Pediatrics recommends adolescent bariatric surgery for those with a BMI that is 120% of the 95th percentile for their age and weight. This recommendation came on the tails of research including one study that found that patients who undergo bariatric surgery maintain an average 29% reduction in BMI at 12 years after surgery.
Indications for bariatric surgery among adolescents and teens include:
- BMI of 40 or greater
- BMI of 35 with a weight-related comorbidity
Despite positive results and millions of teens living with obesity, surgeons perform fewer than 2,000 bariatric procedures on adolescents each year. This puts children at a distinct disadvantage, as earlier intervention leads to improved outcomes.
“[Children are] really fragile early on [when] they’re developing their psychology,” Dr. Atwa says. “You want to catch [and treat obesity] before [children] go into high school or college, [to help] when they’re still developing.”
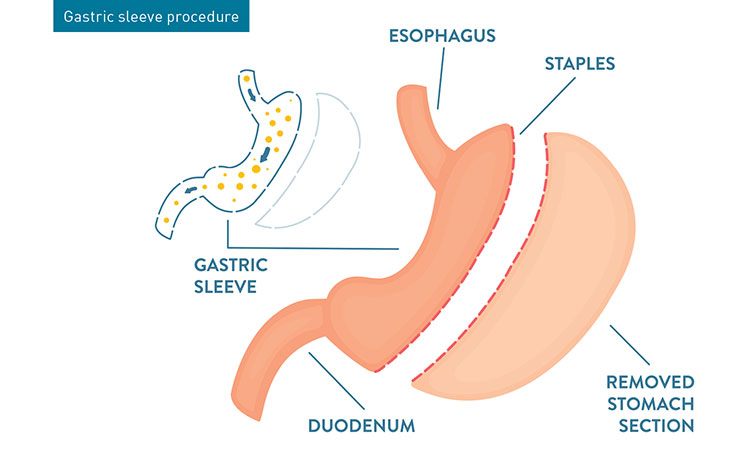
One reason there are so few surgeries is the dearth of available surgery centers that offer adolescent bariatric surgery. St. Charles Hospital in Port Jefferson, where Dr. Atwa serves as Director, Chief of Surgery and Director of Robotic Surgery, is one of the few hospitals in New York offering the procedure. There, Dr. Atwa and Long Island Laparoscopic Doctors offer bariatric surgery for patients as young as 14. (The method of choice is robotic sleeve gastrectomy.) By this age, most children’s bones and growth plates have completed development. Also, the patient is mature enough to follow post-surgical instruction to help ensure success.
While surgery is available starting at age 14, evaluation and education often begin six months prior to turning 14. Because a successful procedure depends on a stable support system, the six-month prep period enables providers to see the child’s support system in action. Providers also have the opportunity to educate patients on lifestyle changes bariatric surgery demands and allow for specialty evaluation. At St. Charles Hospital, a multidisciplinary team follows patients throughout the process. Prior to surgery, pediatricians, pulmonologists, cardiologists and psychologists each sign off on the health and fitness of a given adolescent candidate.
The Next Steps in Obesity Care
Nationwide, adolescent bariatric surgery yields 80%–85% success rates, notes Hesham Atwa, MD, FACS, FASMBS. Within his practice, however, 90% of patients find success.
Though sleeve gastrectomy provides excellent results in the obese adolescent population, Dr. Atwa admits that the ideal solution is not intervention. Rather, it is obesity prevention, which may exist in the near future. Such preventive measures are likely to result from the following two developments:
- Determining and eliminating the toxin that is responsible for the genetic disposition for obesity.
- Genetic testing to identify those children at risk for adolescent obesity and taking steps to monitor and treat them in a timely manner.
Additionally, other therapies hold promise of providing alternatives to surgical intervention. Currently, researchers are working to determine the efficacy of diabetes medication to aid in weight loss. Should this prove fruitful, surgical intervention may become unnecessary. Until then, bariatric surgery remains the greatest therapeutic intervention available to obese adolescents.
To ensure maximum benefit, ongoing support is vital. Dr. Atwa finds that those who enjoy the greatest long-term weight loss take advantage of a support group with fellow surgery patients and have a strong support system at home.
Surgically Induced Success
With a 45-minute procedure, young, obese individuals take a significant step forward, potentially eliminating many common health issues associated with obesity. Previously, researchers thought this weight loss was due to the smaller stomach left behind after bariatric surgery. More recent research has indicated a deeper source of weight loss.
“The reason dieting is .05% successful is because when you’re dieting, your brain says you’re hungry,” Dr. Atwa says. As a result, many fail when relying on diet alone. “[Compare that] to bariatric surgery, where there is a significant decrease in hunger.”
Though the precise mechanism remains a mystery, successful surgery redirects or otherwise interferes with the neurohormonal pathway that decreases the amount of ghrelin hormone and increases the GLP1 (Glucagon-like peptide 1) and PYY (peptide YY) hormones. This hormonal reconfiguration leads to appetite control and weight loss.
Though the mechanism by which adolescent bariatric surgery succeeds is not yet completely understood, the results are consistently positive. To date, the procedure has a 0% mortality rate among adolescents. Comorbidities are typically resolved or prevented in the first place. Teens have renewed self-confidence and energy.
Such results have helped push many pediatricians toward acceptance of the procedure. For obese children, the same is often true. When family members or friends undergo bariatric surgery to positive results, obese adolescents see what changes are possible. Because of the consistently good outcomes, the number of adolescent procedures Dr. Atwa performs each year is increasing. This trend is likely to continue.
“When young patients come to us, they want it done yesterday,” Dr. Atwa says. “They can’t wait to get the operation.” When asked how their lives have changed since surgery, the answer is the same. “They say everything is better, that they should have done it a long time ago.”
As the medical community gains a better understanding of the need and benefit of adolescent bariatric surgery, pediatricians will become more likely to refer patients for the procedure. This is the starting point of a future in which more adolescents and teens avoid a life of obesity and its inherent complications.
Visit JourneyToTheNewYou.com to learn more about Long Island Laparoscopic Doctors.
Source: MD News March 2022, Long Island Edition
