By Robin Overbay
Though the term may sound novel, diabesity is defined by Merriam-Webster as “obesity associated with diabetes.” The surgeons at Long Island Laparoscopic Doctors are highly familiar with both the condition and the surgical treatment of diabesity, which has proven to be superior to pharmacotherapy and less risky than several routine laparoscopic surgeries in various studies.

Diabetes and obesity affect a large portion of people worldwide. Projections show that by 2030, half of the U.S. population will be obese and 25% will have severe obesity. Diabetes affects 10% of Americans, and the CDC reports that 26.8% of adults 65 and older have diabetes. Additionally, 90% of those with Type 2 diabetes are obese or overweight, supporting a strong association between obesity and Type 2 diabetes.
Obesity and diabetes are associated with significant morbidity and mortality. Obesity is the second-leading modifiable risk factor for premature death behind smoking. Due to cellular changes and cytokine production creating a chronic inflammatory state in response to insulin resistance and excess adipose tissue, diabesity can increase the risk of developing various other life-threatening or debilitating conditions. Diabesity increases the risk of macrovascular and microvascular diseases and cancer, including cardiovascular disease, stroke, nephropathy, retinopathy, cognitive impairment, erectile dysfunction, peripheral vascular disease and amputations.
Diabesity: A Modifiable Risk Factor
With bariatric surgery, Type 2 diabetes and obesity are preventable and often reversible, according to metabolic and bariatric surgeon Hesham Atwa, MD, FACS, FASMBS, Founder and Clinical Director of Long Island Laparoscopic Doctors, Director and Chief of Surgery and Director of Robotic Surgery at St. Charles Hospital, and Chief of General Surgery at Mather Hospital Northwell Health. The main advance over the past two decades is the incredible safety profile of bariatric surgery.
Randomized controlled studies support this assertion. Metabolic/bariatric surgery reduces the risk of:
- Atrial fibrillation (22%)
- Cancer (37%)
- Coronary artery disease (20%)
- Heart failure (62%)
- Myocardial infarction (40%)
- Nephropathy (45%)
- Premature death (41%)
- Stroke (42%)
Patients who underwent metabolic surgery and subsequently managed to control their blood glucose for a decade after surgery experienced an even greater reduction in risk of cancer: 60%.
Protection Against COVID-19 Complications
Bariatric surgery also reduces the risk of complications or death from COVID-19. People with diabetes are more likely to have serious complications from COVID-19, including sepsis and septic shock, according to the American Diabetic Association. And obesity triples the risk of hospitalization from a COVID-19 infection, according to CDC statistics. Metabolic/bariatric surgery addresses both these risk factors — a study in JAMA Surgery found that people who had previously had bariatric surgery and later caught COVID-19 had 60% less risk of severe disease and 63% less need for supplemental oxygen.
Diabesity Treatments
Treatment options for diabesity include:
- Lifestyle changes, such as diet and exercise
- Pharmacologic treatment of diabetes, including insulin and oral hypoglycemic and GLP-1 agonists. GLP-1 agonists can also aid in weight loss.
- Pharmacologic treatment of obesity, including traditional weight loss medications and Plenity, a new hydrogel pill made of plant-derived cellulose that expands up to 100 times its size to increase satiety. Plenity was FDA approved for patients with a BMI of 25–40 in 2019.
- Non-invasive procedures like the Orbera balloon, which is placed in the stomach endoscopically for a temporary period of six months. Patients lose an average of 20–50 pounds, and the balloon can be used in conjunction with other weight loss medications.
Metabolic bariatric surgery offers several laparoscopic options that are increasingly safe surgical treatments of diabesity. The most common surgeries are the following:
- Sleeve gastrectomy
- Roux-en-Y gastric bypass
- Biliopancreatic diversion (duodenal switch)
- Single-anastomosis duodenal ileostomy with sleeve gastrectomy (SADI-S)
Surgery Compared to Traditional Approaches
Metabolic/bariatric surgery is the most effective treatment for patients with diabesity. For patients with controlled diabetes, remission following surgery is more likely, with 97% of people with diet-controlled diabetes achieving remission, along with 87% of those on oral medications. Earlier surgical treatment improves outcomes of patients with diabetes and obesity, particularly in patients who have had diabetes for five years or less, according to Dr. Atwa.
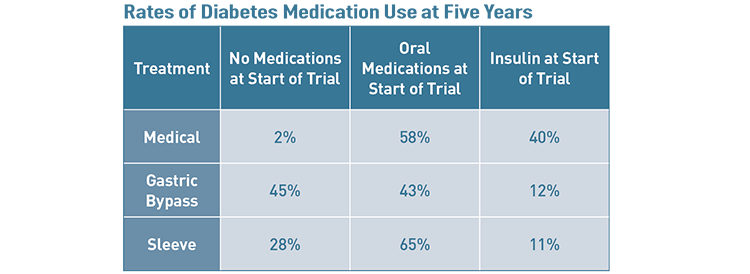
The STAMPEDE trial demonstrated the superiority of surgery over traditional medical management of diabetes at five years in patients with advanced diabetes.
“When they compared surgery to medications, they found that the medical therapy group had to increase medications and the surgical group was able to cut down or eliminate medication,” Dr. Atwa says.
Of course, success varies between individual cases. Factors that impact the success of metabolic surgery for diabetes and obesity include age, percentage of excess weight lost, HbA1c levels, insulin use prior to surgery and duration of diabetes. (See table below for more detail about factors that impact which patients will still need diabetes medicine after treatment.)
Low-Risk Surgery to Reduce Future Higher-Risk Surgeries
Metabolic/bariatric surgical techniques have advanced significantly over the past couple of decades, resulting in an impressive safety profile. For example, the rate of complications following Roux-en-Y gastric bypass is 3.4%, lower than several other laparoscopic procedures including appendectomy (4.5%) and cholecystectomy (3.7%). When compared to surgeries for common complications of diabesity, such as coronary artery bypass graft surgery (46.6%) and infrainguinal bypass (23.6%), the safety of metabolic/bariatric surgery is markedly superior. Of 28 observational studies, all showed reduced mortality following surgery, with an average of 45% risk reduction.
To Refer or Not to Refer?
EscapeDiabetes.org can assist in risk stratification for patients or clinicians. By factoring in certain biometric data, such as age, comorbidities, medications, blood pressure and lab values, this tool estimates the risk of developing certain complications of diabetes and how that risk could change with metabolic bariatric surgery. This may aid in decision-making for those considering consultation for surgery.
Destigmatizing Metabolic Bariatric Surgery
For a lot of people, inability to achieve a normal BMI is not due to lack of effort. Some people have a genetic predisposition to obesity; despite trying numerous diets, they have difficulty losing weight by conventional means. The extra weight obese patients carry also makes exercise difficult and can contribute to significant joint pain.
“Metabolic bariatric surgery should not be viewed as taking the easy way out,” Dr. Atwa says. “Instead, choosing surgery is taking the healthy way out.”
There is a huge opportunity to help patients with diabesity, as currently only 1% of patients who qualify for metabolic/bariatric surgery have had the procedure. With his multidisciplinary team and compassionate approach to diabesity, Dr. Atwa hopes to positively impact more patients and help them live longer, healthier, happier lives. For patients with diabesity, early referral is key to glycemic control or diabetes remission. An hour of surgery can lead to a lifetime of health.
In addition, primary care physicians and endocrinologists may find diabetes and associated comorbidities much easier to manage when they can confidently recommend bariatric surgery as a safe and effective treatment for their patients.
“We have an extremely safe track record and we support each patient fully throughout the weight loss journey,” Dr. Atwa says. “Our patients love us.”
Please visit JourneyToTheNewYou.com to learn more about the services offered at Long Island Laparoscopic Doctors.
Source: MD News April 2022, Long Island Edition
