By Elesa Swirgsdin

For some patients, obesity can recur after bariatric surgery. The team at Long Island Laparoscopic Doctors offers multiple treatment options, including revisional surgery.
Hesham Atwa, MD, FACS, FASMBS, is committed to helping patients with chronic obesity overcome obstacles and live healthier lives. Often, this begins with helping them understand that contrary to popular belief, being obese or having a recurrence after treatment is not their fault.
“It’s important to take the blame away from the patient,” says Dr. Atwa, who is Founder and Clinical Director of Long Island Laparoscopic Doctors, Director and Chief of Surgery and Director of Robotic Surgery at St. Charles Hospital, and Chief of General Surgery at Mather Hospital Northwell Health. “Obesity is a chronic disease. When we treat somebody for cancer and the cancer comes back, we don’t say that we’re not going to do anything else because we failed. We attack it again. It’s the same with obesity. It can be in remission and come back, and we’re going to treat it again.”
Understanding Chronic Obesity
Obesity is a complex condition that can have many possible causes. While poor diet and insufficient physical activity play a big role, other factors, including genetics, are important contributors.
“People can try to change their eating habits, but the rest is up to their body and genetics,” Dr. Atwa says. “The body’s signals control the appetite and tell you when to put down the fork and stop eating.”
This means that many patients who try to lose weight and keep it off with lifestyle changes alone are often unsuccessful. Additionally, weight loss surgery sometimes does not produce the desired results, due to the treatment being ineffective or the patient being a partial or nonresponder.
Research has shown that various genetic factors, including signaling from glucagon-like peptide-1 receptors (GLP-1R), may play an active part in a person’s ability to maintain successful weight loss.
“One study showed that responders are people whose GLP-1R levels go up when they eat, making them feel full,” Dr. Atwa says. “In nonresponders, their GLP levels do not go up as high, so they still feel hungry and eat more.”
Studies have also revealed that nonresponders often have higher insulin resistance than responders, as well as different hormonal responses to glucose.
Finding the Best Treatment Options for Each Patient
In general, a bariatric surgery is considered unsuccessful when a patient meets any of the following criteria:
- Weight loss of less than 50% of excess weight
- Lack of comorbidity resolution
- Low quality of life due to obesity or post-op complications such as new or worsened acid reflux
- BMI higher than 40
When the first surgery does not produce the desired results or the weight comes back over time, each patient is evaluated to determine why the first surgery was not successful before determining the best treatment options going forward.
“We start from the beginning and make sure the patient is exercising and eating healthy,” Dr. Atwa says. “The patient also sees a nutritionist and a psychiatrist to make sure there are no unresolved psychological issues that are contributing to obesity.”
In addition to following a healthy diet and exercise program, weight loss medications can help some patients lose weight without having surgery. GLP-1R agonist therapies have proven to be effective for some people.
Dr. Atwa also stresses the importance of attending monthly support groups.
“We recommend that people attend the support group for the rest of their life,” he says. “We have found that people who attend regularly lose more weight and have a better chance of keeping it off.”
Dr. Atwa says learning about the mistakes other people have made after surgery, as well as hearing about their positive experiences, can be very helpful. “People can share their successes and struggles, and when they see the benefits of the group, they want to keep coming back.”
When noninvasive measures fail, Dr. Atwa recommends revisional surgery for some patients. While revisional surgeries have a slightly higher complication rate, most can be performed robotically, minimizing risk. About 80% to 90% of these surgeries are successful.
Revisional Surgery Options
About 10% to 15% of the bariatric surgeries Hesham Atwa, MD, FACS, FASMBS, Founder and Clinical Director of Long Island Laparoscopic Doctors, performs are revisional procedures. The type of surgery he recommends for each patient depends on several factors, including the original type of procedure the patient had and the reasons it was not successful.
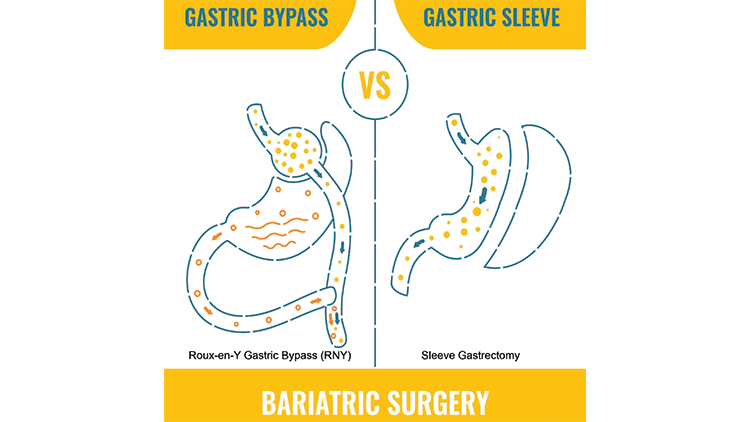
Sleeve Gastrectomy
The most common type of bariatric surgery, sleeve gastrectomy has a revision rate of about 20%. For weight regain, revision options include:
- Re-sleeve if the sleeve is diffusely dilated or there is segmental dilatation with a retained fundus
- Conversion to a gastric bypass
- Conversion to a single anastomosis duodeno ileostomy
For acid reflux, options include gastric bypass; re-sleeve; radiofrequency ablation and augmentation of the lower esophageal sphincter; implantation of a magnetic sphincter augmentation (LINX device); ligamentum teres cardiopexy (“Sling”); and hiatal hernia repair.
Gastric Bypass
Several options are available for patients who had gastric bypass, including pouch and anastomosis reduction, revision of the anastomosis for marginal ulcers or gastrogastric fistula or stricture, and distalization of the alimentary limb to increase the malabsorption effect.
Gastric Banding (Lap-Band)
While the Lap-Band procedure was once the most popular bariatric surgery, it now makes up less than 1% of bariatric surgeries due to its 40% revision rate. If the band has eroded, it must be removed. In the case of prolapse or band slippage, the band may be removed or repositioned. If the patient has experienced inadequate weight loss, the procedure can be converted to a sleeve or bypass after removal of the Lap-Band.
“Most people are very happy,” Dr. Atwa says. “But surgery is not meant to replace healthy nutrition, healthy lifestyle and exercise. It is only done when other treatments have not been successful or if there is an anatomical problem.”
To learn more about bariatric surgery options at Long Island Laparoscopic Doctors, visit journeytothenewyou.com.
