By Elesa Swirgsdin
As robotic surgery evolves, Hesham Atwa, MD, FACS, FASMBS, and Long Island Laparoscopic Doctors offer patients an expanded array of minimally invasive surgical techniques that yield shorter recovery times, fewer complications and reduced post-procedural pain.

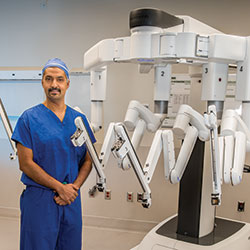
Hesham Atwa, MD, FACS, FASMBS, is at the forefront of minimally invasive robotic-assisted surgery. As the Founder and Clinical Director of Long Island Laparoscopic Doctors, as well as the Director and Chief of Surgery and Director of Robotic Surgery at St. Charles Hospital and Chief of General Surgery at Mather Hospital Northwell Health, Dr. Atwa has experienced firsthand how robotics are changing the face of surgery — for patients and physicians alike.
“Results of robotic-assisted surgery are significant when compared with results of open or laparoscopic surgery,” Dr. Atwa says. “There is a lower rate of complications and a lower death rate. For physicians, this is the next stage of the evolution of surgery.”
Dr. Atwa now has access to five da Vinci System robots, which he uses for colon resections, hernia repairs, foregut surgery, biliary surgery and bariatric surgery. Over the past two years, he has performed more than 850 robotic-assisted surgeries with superior patient outcomes.

Advantages and Advances
The field of robotics advances rapidly. Dr. Atwa’s dedication to mastering those advances means his patients now have options that were unavailable a few years ago. Many surgeries are becoming less complicated, allowing patients to resume their lives faster, with lower chances of returning to the hospital.
“Complications can create the need for prolonged hospital stays and time away from work and family,” Dr. Atwa says. “The benefits that I have seen with robotic-assisted surgery as compared to laparoscopic or open procedures include fewer leaks, blood transfusions, ICU admissions, hospital readmissions and visits to the emergency room, as well as cost savings.”

Another significant advantage of robotic-assisted surgery is the reduced need for prescription opioids.
“Patients have less pain [after surgery],” Dr. Atwa says. “Many people only use over-the-counter pain relievers, or they only need a few prescription pills instead of 30. There’s less chance of becoming addicted to opioids. With overdose death due to opioids up 54% in 2020 for a record 93,000 people, reducing exposure to opioids makes a difference.”
Patients are not the only ones who benefit from robotic surgery. The use of robotic assistance provides surgeons many advantages over both open surgery and minimally invasive laparoscopic procedures.
“Robotics help increase skill level by 15% to 20%,” Dr. Atwa says. “Surgeons can be more precise, more comfortable and have less fatigue.”
Robotic-assisted surgery removes many of the limitations of laparoscopic procedures. While laparoscopy offers some of the same benefits to patients, such as shorter hospital stays, it can be more challenging for surgeons, as it uses 2D imagery and limits the surgeon’s movements.
During robotic-assisted procedures, the surgeon manipulates the robot’s arms while seated at a console that offers a 3D view of the surgical site magnified 10 times. Incorporating tremor-filtration technology and wristed instruments, the robot allows the surgeon to use precise movements with a much greater range of motion than the human hand. Surgeons experience reduced arm, finger and hand fatigue and better dexterity, which leads to higher accuracy and faster surgery completion times.

Colon Resection
Dr. Atwa is a leader in performing robotic-assisted colon resections, which are done to treat chronic or recurrent diverticulitis, cancer, and large polyps that cannot be removed during a colonoscopy. This surgery has traditionally been performed as an open procedure.
A Hour of Surgery, a Lifetime of Difference
A simple, safe and precise procedure that takes less than an hour to perform will help obese patients lose 1/3 or more of their weight, resolve most if not all their medical problems, and enable them to feel and look better.
“More than half of colon resections in the U.S. are still done through an open surgical procedure,” Dr. Atwa says. “When colon resections are performed as an open surgery, patients are at higher risk for infections and hernias, and they stay in the hospital longer. It takes about six to eight weeks to recover because of the larger incision.”
About 95% of the colon resections Dr. Atwa performs are now robotic-assisted procedures. Using da Vinci’s integrated Firefly fluorescence imaging capability, he can visualize and evaluate the blood supply of the remaining colonic segment more effectively than with the naked eye, which dramatically reduces complications.
“Patients can now go home faster than before, usually within one to two days instead of three to five days,” Dr. Atwa says. “They have less pain and can return to their normal activities faster.”
Mather and St. Charles Hospitals are two of only a few hospitals to offer robotic surgery 24/7. As a result, patients are able to receive the very best surgical option regardless of the time of day.

Improved Hernia Repair
While open surgery for hernia repair is still common in the U.S., with about 60% of procedures performed in the conventional method, Dr. Atwa performs many hernia repairs robotically, including all inguinal, incisional and ventral hernias.
“We have had very few recurrences,” he says. “Most patients go home the same day. Inguinal hernia surgeries usually take about a half an hour. In the case of a bilateral hernia, the procedure takes an extra 10 minutes.”
In addition to the benefits associated with robotic surgery — reduced complications, with fewer infections and shorter recovery times — hernia surgeries have become more advanced in other ways in recent years. For example, because using tacks to secure surgical mesh could cause post-operative complications as well as increase costs, surgeons now use self-gripping mesh or sutures.

Foregut Surgery
For patients with symptomatic hiatal hernias or GERD that is refractory to medical treatments, as well as patients who prefer surgery over medication, robotic Nissen fundoplication is available at Long Island Laparoscopic Doctors. This procedure reinforces the lower esophageal sphincter and helps prevent acid from backing up into the esophagus.
“Most patients who have this surgery will be able to stop taking long-term acid-reducing medications,” Dr. Atwa says. “Barrett’s esophagus is often resolved or well-controlled as a result, as well.”
Dr. Atwa has also had success in resolving achalasia by performing the Heller myotomy procedure robotically. He notes that this procedure can be life-changing for some people, as many have a marked improvement in their ability to swallow within just a few hours of the surgery.
Biliary Surgery
Laparoscopic cholecystectomy is a common procedure, with 300,000 performed in the U.S. every year. By using robotic assistance, Dr. Atwa can achieve greater precision in performing cholecystectomy, which leads to improved patient outcomes.
Firefly technology helps to visualize the biliary anatomy, allowing for increased dissection accuracy. While with other forms of surgery, obesity can be a barrier to surgery, this advanced technology eliminates weight as an obstacle. It also reduces the frequency of conversions to open surgery.
“Robotic cholecystectomy results in fewer bile leaks, blood transfusions, infections and readmissions to the hospital,” Dr. Atwa says.
Bariatric Surgery
The obesity epidemic continues to be a major issue of concern for multiple reasons. Complications of being overweight or obese rank as the second leading cause of preventable death in the U.S.
“Obesity is a chronic disease that affects more than 60% of the U.S. population,” Dr. Atwa says. “Many patients think it’s their fault, but that is not true. It’s like any other disease — it requires treatment. The problem is that obesity can cut your life by 10 to 12 years, and it causes many other medical problems. This one disease affects almost every organ in the body.”
Obesity can lead to migraines, stroke, heart attack, sleep apnea, acid reflux, fatty liver disease, joint and back pain, diabetes, hypertension, and high cholesterol. People with obesity are also at higher risk for cancer.
Meet Dr. Atwa
Hesham Atwa, MD, FACS, FASMBS, Founder and Clinical Director of Long Island Laparoscopic Doctors, is known across Long Island as an advocate and educator in the field of robotic-assisted surgery, which he uses consistently for both general and bariatric operative procedures. Dr. Atwa is also Director and Chief of Surgery and Director of Robotic Surgery at St. Charles Hospital and Chief of General Surgery at Mather Hospital, a member of Northwell Health.
Dr. Atwa has performed more than 10,000 surgeries and assisted on 6,000 more throughout his career.
Dr. Atwa attended medical school at Ain Shams University in Cairo and completed his residency at the University of Illinois — Metropolitan Group Hospitals in Chicago. He then completed a fellowship in advanced laparoscopic surgery at The University of Texas in Houston.
Though he stays busy with his hospital duties and practice, Dr. Atwa also serves as a proctor for Intuitive Surgical, assessing other surgeons and helping them learn new techniques for robotic surgery.
To better serve his community, Dr. Atwa performs procedures as part of a devoted group of Long Island surgeons who take care of charity cases at the Port Jefferson Surgery Center for patients who don’t have insurance or cannot afford surgery. In 2018, he was named a recipient of the prestigious Theodore Roosevelt Award presented by Mather and St. Charles Hospitals to physicians for exceptional volunteer service to the community and the hospital.
“Despite all the awards and titles, the best compliment and reward is getting a hug after removing a cancer from a patient or having a patient lose 100 pounds after dieting and exercising for years without success,” Dr. Atwa says. “I feel one of the highest honors in medicine that I have received is to be asked to take care of my colleagues at the hospital, whether it be doctors, nurses, hospital staff or their families. I provide every patient my very best care as if they were a member of my own family.”
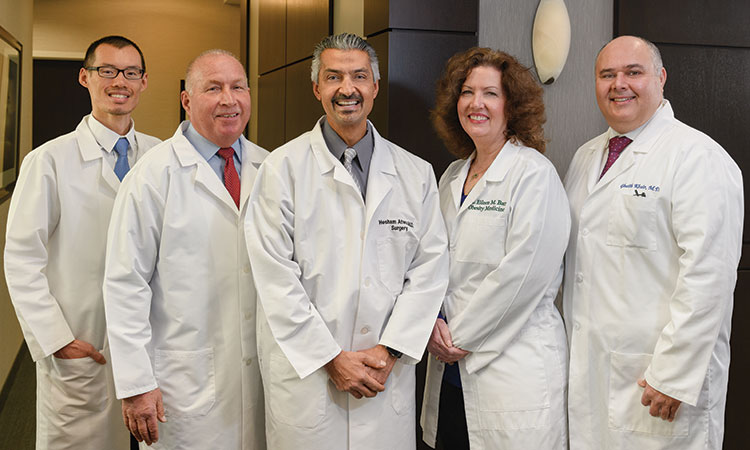
Meet the Long Island Laparoscopic Doctors
- Eileen M. Barr, DO — Obesity medicine physician
- Jon Leung, DO, FACOS — Minimally invasive general and bariatric surgeon
- Ghaith Khair, MD — Minimally invasive general and bariatric surgeon
- Nicholas P. Craig, MD, FACS — Minimally invasive laparoscopic general surgeon
“Let’s not forget the lessons of the COVID-19 pandemic,” Dr. Atwa says. “According to the CDC, more than 70% of COVID-19 patients in the U.S. who were hospitalized were overweight or obese. Having bariatric surgery can cut down that risk.”
Dr. Atwa notes that many patients tell him they feel like a failure when they lose weight and gain it back again.
“I tell them ‘Obesity is not a sign that a person is out of control,’” he says. “Many things can contribute to this condition. It’s no wonder that the long-term success of diets is only 0.05%.”
Long Island Laparoscopic Doctors offers several options for bariatric surgery, all of which are available as robotic procedures. These include gastric bypass, gastric sleeve, revisional bariatric surgery, gastric band revision surgery and adolescent bariatric surgery.
Adolescent obesity is on the rise. Recognizing that earlier treatment allows most medical problems to resolve, Long Island Laparoscopic Doctors accepts patients as young as 14 years old. A 60-second assessment is available for patients on the practice’s website to help people determine whether they are ready for surgery and which type might be the best choice.
“After surgery, most patients report more energy, less fatigue, more mobility, better sleep, and less joint and back pain,” Dr. Atwa says. “They also have better self-esteem and are able to do activities they couldn’t before, like play with their kids. Surgery changes their lives.”
For patients who don’t qualify for or don’t want to undergo surgery, nonsurgical treatments are also available, including the Orbera gastric balloon. But Dr. Atwa adds that for all options, patients must also follow an exercise program and adjust their eating habits for the weight to stay off.
“If patients are struggling, they can come to us and review their options,” he says. “It’s a chronic disease, and if it comes back, we can determine the reason and deal with it.”
Partners in Advanced Care
Dr. Atwa encourages referring physicians to explore the advanced surgical options available for patients who could be candidates for bariatric surgery. He and his colleagues at Long Island Laparoscopic Doctors partner closely with primary care physicians, endocrinologists and gastrointestinal physicians to determine the best course of treatment for patients and get them on the road to a healthier and happier life.
Long Island Laparoscopic Doctors has two convenient locations, in East Setauket (4 Technology Drive, Suite 220, East Setauket, NY 11733) and Commack (500 Commack Road, Suite 150D, Commack, NY 11725). In addition to St. Charles and Mather Hospitals in Port Jefferson, Long Island Laparoscopic Doctors’ surgeons see patients at Peconic Bay Medical Center in Riverhead, St. Catherine Hospital in Smithtown, and Huntington Hospital.
Both St. Charles and Mather Hospitals are among a special group of hospitals that belong to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program – Centers of Excellence for Bariatric Surgery. They rank among the top hospitals in the U.S. for bariatric treatment. St. Charles is also one of the few epicenters for bariatric, colorectal and general surgery where surgeons can come in to observe and learn new techniques to add to their practice.
“Through the years, I have been extremely fortunate to be able to associate myself with a talented group of providers and surgeons across Long Island,” Dr. Atwa says. “We constantly turn to each other for consultations about treatment options for our patients and collaborate on rare or challenging cases. While I retain the independence of a physician in private practice, I am privileged to work within hospitals committed to staying at the forefront of advanced technology to provide optimal outcomes for our patients and communities. At our offices and in our hospitals, we share one vision — to treat patients as we’d want our own families to be treated.”
The Life-Changing Benefits of Bariatric Diabetes Surgery
The combined epidemics of obesity and diabetes have been referred to as “diabesity,” something that has become a profound concern due to the health risks of having both conditions.
“For a lot of patients, diabetes and obesity go hand in hand,” says Hesham Atwa, MD, FACS, FASMBS, Founder and Clinical Director of Long Island Laparoscopic Doctors.
The cost in suffering is immense. Every year, 79,535 deaths occur due to diabetes. There are approximately 150,000 nontraumatic leg amputations every year in the U.S., and the leading cause is Type 2 diabetes.
Fortunately, bariatric surgery can be a significant remedy for diabetes.
“Even if surgery doesn’t eliminate the diabetes one hundred percent, it makes it more manageable and helps prevent the progression, before it affects organs like the eyes and the kidneys,” Dr. Atwa says. “Some people might be able to take just one or two medications instead of five or six to control the disease.”
The Evidence In Support of Bariatric Surgery for Type 2 Diabetes Continues To Mount
- 77% of patients with resolved diabetes. In these patients, diabetes completely disappeared, or treatment (medicines, insulin) was no longer needed. In studies measuring for “resolution or improvement,” the number rose to 86% of patients.
- Rapid results. For some patients, diabetes disappeared almost immediately, within days of surgery. Others saw blood sugar levels begin to fall soon after surgery, becoming completely normal within a year.
- 92% reduction in deaths. In one study of 15,850 severely obese patients, those who underwent bariatric surgery had a 92% lower rate of death from diabetes than those who didn’t have the surgery.
To learn more, visit journeytothenewyou.com.
