By Jennifer Robinette
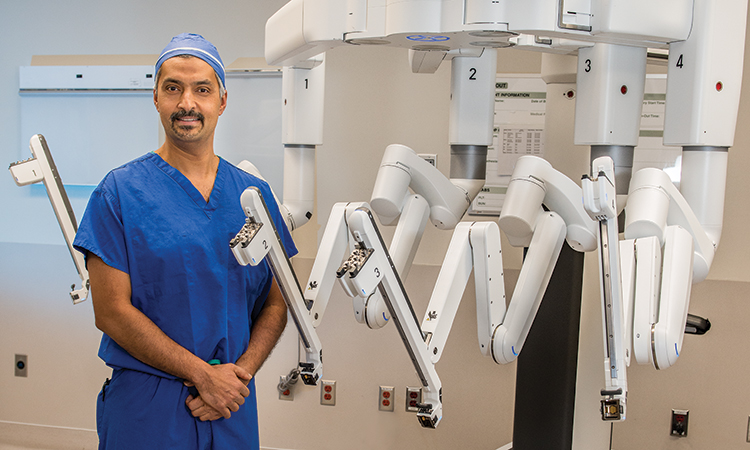
Robotic surgery is the next level in the evolution of modern surgery, as Hesham Atwa, MD, FACS, FASMBS, can attest.
“Surgery has evolved over the years,” he says. “Thirty years ago, we were doing procedures as open surgery. Then 25 years ago, laparoscopic surgery became an option. Over the past five years, robotic surgery has improved on those techniques.”
Dr. Atwa is Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at John T. Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors. He performs most of his procedures using robotic surgery techniques. He explains that new technologies have revolutionized surgery over the past five years — and his patients are benefiting from them.
During his time as a proctor for Intuitive Surgical’s da Vinci surgical systems, Dr. Atwa has witnessed a marked increase in the variety and precision of procedures performed robotically. The precision of robotic surgery provides improved patient outcomes and significantly shortens recovery times.

General Advantages to Robotic Surgery
Robotic surgery provides many advantages to the surgeon who employs this technique. Surgeons perform robotic procedures while seated; as such, they benefit from an ergonomically aligned position that can make a long or complex operation less tiring.
“The technology cuts down on fatigue, which is a common cause of medical errors,” Dr. Atwa says.
The robot also increases surgical control as it provides a magnified, high-definition view of the operative field. According to Dr. Atwa, operating with the robot enhances a surgeon’s dexterity, as its wristed instruments allow the operator to be more precise than with standard instruments. Physicians who perform robotic surgeries can expect a 15–20% improvement in their skill level. Robotic surgery provides advantages to patients as well as the surgeons who care for them. Robotic improvements minimize patient size as a barrier to surgery. Smaller incisions and more precise surgical techniques translate into shorter recovery periods and reduced need for pain medications. Reducing the number of opioid prescriptions helps combat the current opioid crisis.
“Before, I might have prescribed 30 opioid pills to help a patient recover from surgery,” Dr. Atwa says. “But the robot cuts down pain. In many cases, I can write five pills for the patient, and they might take two or three of them.”
Patients who have robotic procedures generally return to work faster, have fewer infections — and see better cosmetic results.

Robotic Surgery for Colon Resection
Dr. Atwa is one of the first surgeons on Long Island to perform colon resections without any stapling. He accomplishes this by removing the diseased portion of the colon through a natural orifice. This puts him on the leading edge of minimally invasive colon surgeries.
Dr. Atwa prefers robotically assisted colon surgery because it allows an advanced degree of precision when evaluating the blood supply to and limits of intended resection.
He explains that “articulation and rotation of the instruments allows safe resection and obtaining difficult angles.”
With da Vinci’s Firefly Fluorescence Imaging technology, the surgeon can visualize the blood supply of the remaining colonic segment that is not always apparent to the naked eye. Using these tools reduces the risk of leaks and abscesses and decreases the overall complication rate.
The result, Dr. Atwa explains, is an expedited recovery for the patient and a minimized risk for developing delayed complications such as hernias or infections. Colon resection using this technique is still uncommon across the United States.
“Half of colon resection procedures in the U.S. are performed as open surgeries,” Dr. Atwa says. “However, I perform 90% of my procedures using the minimally invasive technique.”

New Guidelines for Bariatric Surgery in Adolescents
The American Academy of Pediatrics (AAP) recently released new guidelines for physicians treating adolescents living with obesity and related health issues. The guidelines stress the appropriateness of bariatric surgery for some adolescents and help practitioners determine which adolescents might benefit from surgical treatment.
The guidance, Pediatric Metabolic and Bariatric Surgery: Evidence, Barriers, and Best Practices, was published on Oct. 27, 2019. The AAP guidelines will help pediatricians and other practitioners identify eligible patients and work with their families to prepare them for the procedure and the necessary lifestyle changes.
An accompanying document, Metabolic and Bariatric Surgery for Pediatric Patients with Severe Obesity, is also available now. According to the AAP, it outlines procedure options, outcomes and possible complications relating to surgical intervention.
Hesham Atwa, MD, FACS, FASMBS, Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at John T. Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors, is encouraged by these new guidelines — especially given the rising number of adolescents living with obesity.
“The CDC notes that the percentage of U.S. children and adolescents affected by obesity has tripled since 1970,” Dr. Atwa explains. “In a recent study, Teen-LABS [Teen Longitudinal Assessment of Bariatric Surgery], teenagers who underwent gastric bypass or sleeve gastrectomy lost on average 27% of their weight and saw the resolution of many comorbidities. Teens living with Type 2 diabetes saw the conditions resolved 95% of the time. Those living with hypertension had resolution of the condition 74% of the time.”
Dr. Atwa hopes physicians treating eligible adolescents will refer them for further care.
“This surgery is an effective treatment for diabetes and obesity-related diseases, and the earlier you can intervene in patients’ lives, the better the results you can achieve,” Dr. Atwa says. “Additionally, it can help teenagers with their social development.”
Robotic Surgery for Hernia Repair
In the United States today, more than half of hernia repairs are performed using the open surgery technique. But it is possible to repair inguinal, incisional and umbilical hernias using robotic technology and techniques.
“The robot gives the surgeon more confidence because of its magnified 3D high-definition capabilities,” Dr. Atwa explains. “It also allows a deeper view to reach and dissect the surrounding areas around the hernia defect. This allows for better coverage of the mesh over the hernia space.”
In the past, surgeons placed tacks to hold surgical mesh in place following hernia repair, but, Dr. Atwa says, they could be a source of post-operative pain and increased costs.
“Now we use mesh that is self-gripping or only needs a suture to hold in place, which is less painful and more cost effective,” he says.
Dr. Atwa has seen firsthand the positive impact robotic hernia repair can have in the lives of his patients. He was able to repair a bilateral inguinal hernia in an 86-year-old female patient in 45 minutes. That patient, he adds, was able to leave the hospital less than two hours after the procedure and did not need any postoperative opioid pain medication.
For male patients, robotic hernia repair offers the added benefit of protecting testicular vessels and nerves. This can greatly increase the patient’s postsurgical quality of life.
“With more precise dissection, the surgeon is able to avoid injury to the testicular vessels. With the magnified view, the surgeon can see and avoid injury to the nerves in the area,” Dr. Atwa says.
The incidence of incisional hernia recurrence is also reduced when the procedure is performed robotically. According to Dr. Atwa, “The surgeon is able to sew the defect closed as well as imbricate the diastasis recti — the bulge between the rectus muscle — which helps decrease recurrence of the hernia repair and decrease seroma formation. The surgeon is also able to sew the mesh in place to prevent it from dislodging.”

About Dr. Atwa
Hesham Atwa, MD, FACS, FASMBS, Founder and Clinical Director of Long Island Laparoscopic Doctors, is a leading proponent and educator of robotic assisted surgery for both general and bariatric operative procedures. He is also Director and Chief of Surgery at St. Charles Hospital and John T. Mather Hospital Northwell Health Chief of Surgery and Member at Large of the Medical Board.
Over the past 18 years, he has performed more than 10,000 surgical cases and assisted on more than an additional 5,000.
Dr. Atwa attended medical school at Ain Shams University in Cairo. He completed his residency at the University of Illinois — Metropolitan Group Hospitals in Chicago. Following his residency, he completed a fellowship in advanced laparoscopy at The University of Texas in Houston.
In addition to his hospital duties and practice, Dr. Atwa serves as a proctor for Intuitive Surgical. In that role, he assesses other surgeons and helps them hone their skills. In 2017 and 2018, he was named a recipient of the prestigious Theodore Roosevelt Award presented by Mather and St. Charles Hospitals to physicians for exceptional volunteer service to the community and the hospital. Dr. Atwa is also is one of a select group of Long Island surgeons who perform charity cases at the Port Jefferson Surgery Center for patients who don’t have insurance or can’t afford surgery.
“Despite all the awards and titles, the best compliment and reward is getting a hug after removing a cancer from a patient or having a patient lose 100 pounds after dieting and exercising for years without success,” Dr. Atwa says. “It’s also an honor to be asked to care of my nurse or doctor colleagues and their families.”
Robotic Advances for Foregut Surgery
A wealth of robotically assisted foregut surgeries is available to patients who turn to Long Island Laparoscopic Doctors. For those living with GERD that is refractory to medical treatment, Nissen fundoplication can offer relief. This robotic procedure helps reinforce the lower esophageal sphincter.
Robotic surgery intervention is becoming increasingly more common to resolve hiatal hernia, too. For patients who are symptomatic and need relief, a hernia repair procedure can be done efficiently using a robotic technique.
Patients with achalasia can greatly benefit from the Heller myotomy procedure. This involves relieving the narrowing of the patient’s esophagus by cutting a portion of the lower esophageal sphincter to loosen the muscle and alleviate dysphagia. This option offers fewer side effects and greater long-term success rates for patients than treatment options that were previously available.
“Within a few hours of surgery, many patients notice a remarkable difference in their ability to swallow,” Dr. Atwa says. “This procedure can have life-changing results for certain patients.”

Improvements in Biliary Surgery
Cholecystectomy is a common surgical procedure in the U.S. Approximately 300,000 of the patients diagnosed with gallstones each year undergo the procedure. Robotic technology can improve outcomes and offer an advanced degree of precision for routine procedures like this one, too.
“During cholecystectomy, the robot will visualize normal biliary and aberrant ducts to avoid injuries and leaks,” Dr. Atwa explains. “Firefly technology is used to visualize the biliary anatomy, providing for more precise and accurate dissection. This imaging tool is so precise that it doesn’t matter if the patient weighs 185 lbs. or 485 lbs.”
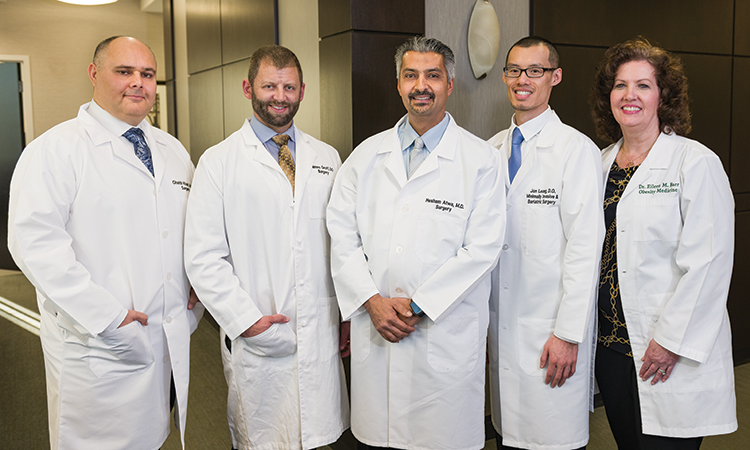
Meet the Long Island Laparoscopic Doctors
Eileen M. Barr, DO — Obesity medicine physician
Jon Leung, DO, FACOS — Minimally invasive general and bariatric surgeon
James L. Groff, DO — General and trauma surgeon
Ghaith Khair, MD — Minimally invasive general and bariatric surgeon
The power of robotic technology is especially helpful when procedures like cholecystectomy present unique challenges.
“I recently performed a cholecystectomy with a fistula between the colon and the gallbladder, which is an extremely rare condition,” Dr. Atwa says, adding that the robot’s assistance eased the procedure.

Bariatric Surgery
The epidemic of obesity in America is of grave concern to doctors and patients alike, accounting for approximately 400,000 deaths and more than $150 billion in medical costs annually.
“Obesity-related complications need to be addressed. Obesity affects 60% of the U.S. population,” Dr. Atwa says. “Morbid obesity increases the risk of cancer and should be treated as such.”
Dr. Atwa and his colleagues at Long Island Laparoscopic Doctors offer surgical solutions for eligible patients. There are several procedure options for bariatric surgery — all of which can be performed using advanced robotic technologies. These include sleeve gastrectomy, gastric bypass, LAP-BAND removal with conversion to a sleeve gastrectomy or bypass, and bypass revision surgery. In cases where a patient doesn’t qualify for weight-loss surgery, doesn’t want a surgical solution or is superobese and needs to lose weight prior to weight loss surgery, Long Island Laparoscopic Doctors also offer nonsurgical treatments, such as the Orbera gastric balloon, and a physician-assisted medical weight loss program.
“Bariatric procedures can take one to two hours to perform, but can completely change a patient’s life,” Dr. Atwa says. “Patients usually stay in the hospital for less than 12–24 hours after the procedure. Then they can go home and begin their new lives.”
“Going from laparoscopic surgery to robotic surgery is like going from a flip phone to an iPhone. You’re adding a computer to your hand, and it can greatly increase a surgeon’s skill and accuracy.”
— Hesham Atwa, MD, FACS, FASMBS, Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at John T. Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors
Barriers to obesity treatment include the personal discomfort physicians and patients feel when discussing the issue and the fear of cost; however, Dr. Atwa encourages other physicians to talk to their patients about the issues surrounding obesity.
“Under current guidelines, about 25 million people qualify for bariatric surgery,” Dr. Atwa says.
He recommends that physicians refer patients who are candidates for treatment, as most insurance plans cover bariatric surgery after an evaluation period.
Advanced Technology for Patients
The hospitals where Dr. Atwa performs his robotic procedures utilize the da Vinci Xi surgical system. Dr. Atwa describes the Xi model robot as “the most advanced on the market today.”
Both St. Charles and Mather Hospitals are among a special group of hospitals that belong to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program – Centers of Excellence for Bariatric Surgery. They rank among the top hospitals in the United States for bariatric treatment.
With the available advancements in modern operating techniques, Dr. Atwa encourages referring physicians to inquire into the options available for their patients who could benefit from weight loss surgery. Long Island Laparoscopic Doctors view gastrointestinal and primary care physicians as key partners. By working together, physicians can improve access and outcomes for their patients. Dr. Atwa and his colleagues work closely with patients’ regular physicians to provide the most appropriate care possible, from advanced surgery to ongoing management and consultation when needed. With offices at two convenient locations, East Setauket (4 Technology Drive, Ste. 220, East Setauket, NY 11733) and Riverhead (806 East Main Street, Riverhead, NY 11901), Long Island Laparoscopic Doctors is easily accessible. In addition to St. Charles and Mather Hospitals in Port Jefferson, Long Island Laparoscopic Doctors’ practice surgeons see patients at Peconic Bay Medical Center in Riverhead, St. Catherine Hospital in Smithtown, and Huntington and South Hampton Hospitals.
“I have been fortunate to work with a group of very talented providers and surgeons in my local area and throughout Long Island. We discuss the various treatment options for our patients and collaborate on difficult or unusual cases,” Dr. Atwa says. “Even though I’m in private practice, I am able to work within hospitals that have the latest technologies to better serve our patients and our community. Our excellent team at our office and in our hospitals treats patients like their own family.”
For more information, visit JourneyToTheNewYou.com.
