By Robin Overbay
Technological advances in medicine have resulted in more versatile and more effective neuromodulation devices that can aid in improved control of various types of chronic pain. NSPC leads the way on Long Island in making these advances available for patients.

Around one-fifth of the adult population in the U.S. reports having experienced chronic pain — defined as persistent pain lasting longer than expected for normal healing — in the past three months, according to the American Pain Society and the International Association for the Study of Pain. Of those patients, more than a third report that chronic pain frequently affects their ability to work. The overall economic burden of chronic pain in the U.S. is estimated to be around $560 billion annually.
The use of opioid medications is common among chronic pain sufferers. With the opioid epidemic persisting in the U.S., it is no surprise that clinicians and patients are looking to other means of pain control. Brian Snyder, MD, a neurosurgeon at NSPC Brain & Spine Surgery, considers the appropriateness of neuromodulation for chronic pain sufferers when other treatments fail. Dr. Snyder is a board-certified and fellowship-trained neurosurgeon and an expert in neuromodulation.
“Neuromodulation is one piece in a very complicated puzzle,” Dr. Snyder says. “But without a doubt, neuromodulation has a strong track record of decreasing patients’ pain and improving their ability to participate in their activities of daily living [ADLs], not to mention helping them reduce narcotic use and stay out of the emergency room.”

Long-Term Effects of Chronic Pain
Chronic pain can be demoralizing to patients, not only impacting them physically but also impacting their mental health, finances, other aspects of physical health and overall quality of life. Living with chronic pain can limit patients physically from being able to work, resulting in missed days of work or permanent disability.
Pain can also affect ADLs and affect patients’ ability to participate in certain social activities. Something as basic as doing household chores or playing with their children can prove very difficult or even impossible for some people with chronic pain.
Chronic pain can often negatively impact patients psychologically, resulting in higher rates of mood disorder, such as depression, anxiety or opioid dependence. Additionally, chronic pain sufferers may have difficulty sleeping due to physical pain and/or psychological impacts of chronic pain. Some studies have shown a negative impact on cognitive function and memory in patients with chronic pain, showing loss of neocortical gray matter on brain scans and changes in brain chemistry. Studies have also shown a link between chronic pain and increased risk for cardiovascular disease, which may be in part due to difficulty performing regular cardiovascular exercise secondary to pain’s negative effect on mobility.
Given the multitude of long-term adverse effects, chronic pain is not something to be ignored. Fortunately, the medical field continues to produce technological advances that could be the answer for these patients as they search for ways to alleviate their pain and regain function.

Hope for People with Pain Refractory to Treatment
While neuromodulation can be life-changing for some, it is not a first-line therapy. Specifically, neuromodulation is reserved for those who have tried and failed other medical treatments appropriate for their conditions. These first-line treatments may include pharmacologic therapy, physical therapy, holistic measures, neuropsychological testing, surgery to correct structural problems, injections and/or ablation.
However, when these therapies fail, innovative neuromodulation devices may provide significant relief. Neuromodulation may sometimes offer modest benefits, which can still make a significant difference in patients’ lives; at other times, it can make a tremendous difference, according to Dr. Snyder.
Conditions Treated
Chronic pain conditions that neuromodulation can treat include but are not limited to:
- Abdominal pain
- Atypical facial pain
- Chronic headache
- Cluster headache
- Complex regional pain syndrome
- Failed back syndrome
- Groin pain
- Intercostal pain
- Perineal pain
- Peripheral nerve injuries or compression
- Peripheral polyneuropathy, such as diabetic- or chemoradiation-induced neuropathies
- Phantom limb pain
- Postherpetic neuralgia
- Post-stroke pain Other conditions that can be treated with neuromodulation include but are not limited to the following:
- Depression
- Dystonia
- Essential tremor
- Incontinence
- Obsessive-compulsive disorder
- Parkinson’s syndrome
- Seizures
- Tourette’s syndrome
Types of Neuromodulation Devices
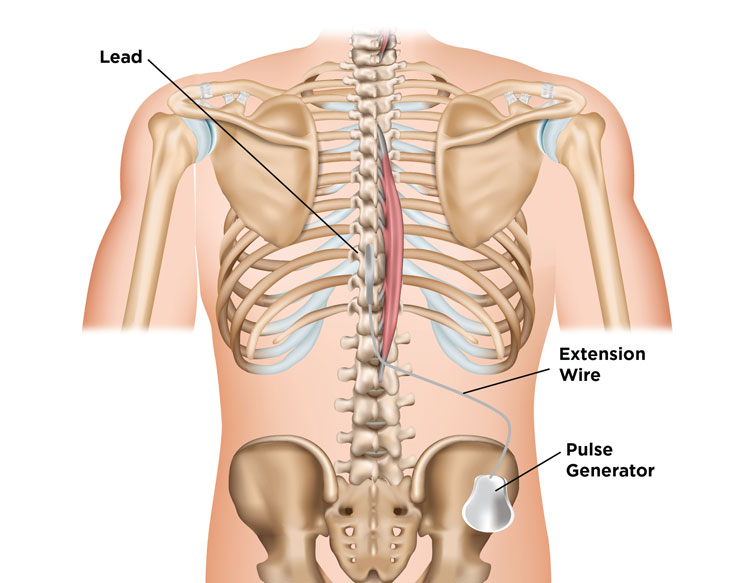
Several types of neuromodulation devices exist on the market today (see “Neuromodulation Devices Available at NSPC”) and may be used for chronic pain refractory to conventional treatments, as well as treating several other medical conditions (see “Conditions Treated”). Most neuromodulation devices require implantation of a neurostimulator device with electrodes placed at the target site. Patients can often control their neurostimulator with a remote device. In general, neurostimulation works by using electrical impulses to interrupt the pain signal to the brain, replacing the perception of pain with a much more tolerable tingling sensation (paresthesia).
However, some newer devices on the market are capable of neurostimulation without perceivable paresthesias for patients who find the paresthesias uncomfortable.
The neurosurgeon typically begins the patient on a trial period with a temporary neurostimulator in order to evaluate efficacy prior to placement of a permanent device.
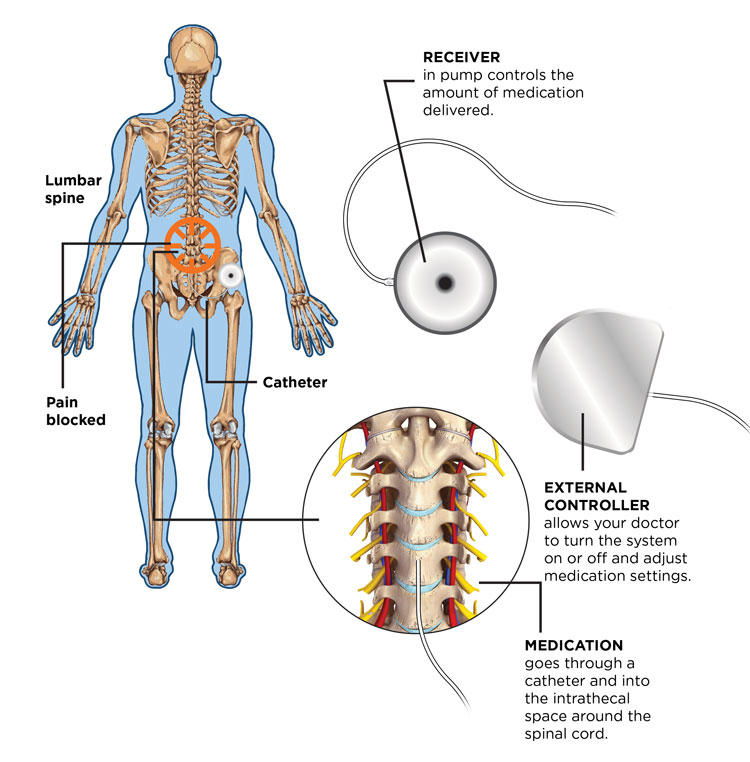
An intrathecal pump is another neuromodulating device that ultimately allows medication to be infused into the intrathecal space, reaching receptors at the target site more efficiently than systemic medications.
“This technology is advancing rapidly,” Dr. Snyder says. “It’s extremely versatile, and there are numerous opportunities to help different patients, as well as multiple interventions that may help any given patient.”
A few of the more commonly used neuromodulation techniques include spinal cord stimulation, dorsal root ganglion stimulation, peripheral nerve stimulation, occipital nerve stimulation, motor cortex stimulation, deep brain stimulation and vagal nerve stimulation.
Spinal Cord Stimulation
Spinal cord stimulation devices may be used for chronic refractory back pain and pain persisting after back surgery. Spinal cord stimulation may also be used for diabetic neuropathy, chemotherapy-induced neuropathy, phantom limb pain following amputation, pain associated with peripheral vascular disease, abdominal pain, perineal pain and other pain syndromes.
Dorsal Root Ganglion Stimulation
Dorsal root ganglion stimulation devices act on the sensory nerves in the dorsal root ganglia of the spinal column. Dorsal root ganglion stimulation may be used for complex regional pain syndrome, extremity pain, groin neuralgia, pelvic pain and other pain syndromes.
Peripheral Nerve Stimulation
Peripheral nerve stimulation devices act directly on peripheral nerves and may be efficacious in patients with pain originating from a peripheral nerve, such as certain compressive neuropathies (nerve entrapment), peripheral nerve injuries and intercostal neuralgias.
Occipital Nerve Stimulation
Occipital nerve stimulation devices act directly on branches of the occipital nerve. The greater occipital nerve provides sensation to the scalp and temporal region. The lesser occipital nerve provides sensation to the ear. Occipital nerve stimulation is a minimally invasive technique in which the stimulator is placed near the cervico-occipital junction. Indications for occipital nerve stimulation include chronic headache (defined as 15 or more headache days per month for more than three months), occipital neuralgia, cervicogenic headache, chronic migraine, cluster headache and hemicrania continua.
Motor Cortex Stimulation
Motor cortex stimulation devices act on the primary motor cortex in the brain. Motor cortex stimulation can be used to treat post-stroke pain, atypical facial pain and other chronic refractory pain syndromes. In investigational applications, motor cortex stimulation has been used to treat other conditions including dysphagia, aphasia, movement disorders and some psychiatric disorders.
Deep Brain Stimulation
Deep brain stimulation devices act on specific areas of the brain to control abnormal brain activity. Deep brain stimulation is most commonly used in non-pain conditions such as Parkinson’s disease, essential tremor, epilepsy, obsessive-compulsive disorder and dystonia.
Deep brain stimulation is rarely used for chronic pain; however, some studies evaluated the treatment of chronic pain with deep brain stimulation for conditions such as phantom limb syndrome, brachial plexus injuries and post-stroke pain. Common target areas in the brain for treatment of chronic pain with deep brain stimulation include the periventricular region and parts of the thalamus.
Vagal Nerve Stimulation
Vagal nerve stimulation devices act directly on the vagus nerve and are more commonly used to treat non-pain conditions, such as seizures. Vagal nerve stimulation devices can also be applied to various chronic pain syndromes, as well as refractory depression.
Intrathecal Pumps
Intrathecal pumps can be used to deliver medications directly to the spinal fluid. Since the medication is delivered straight to the target site, patients may require less medication and may have fewer systemic side effects than they would if they took the medication orally. The intrathecal pump is implanted under the skin at the lower abdomen and attaches to catheters that are directed to the intrathecal space surrounding the appropriate region of the spinal cord.
“We use intrathecal pumps to deliver a range of medications,” Dr. Snyder says. “They can be deployed to deliver medications including narcotics, local anesthetics, baclofen, which has some adjunctive pain relief, and sometimes other drugs. They can be very effective in some neuropathic pain situations.”
Intrathecal pumps deliver medications including but not limited to:
- Opioids, such as morphine
- Non-narcotic pain medications, such as Prialt (ziconotide), a peptide derived from the cone snail that works through inhibition of N-type calcium channels to block nociceptive signals
- Skeletal muscle relaxants, such as baclofen, which may provide some adjuvant pain relief
For patients with chronic, debilitating pain that conservative therapies have failed to manage, consultation with a skilled neurosurgeon who is well versed in neuromodulation devices can help ascertain the most beneficial neuromodulation device for that patient.
“It’s not one-size-fits-all,” Dr. Snyder says. “With our experience, we can hope to find the optimal target and the optimal device for the ideal outcome.”
Revision Surgeries
Patients with existing implanted neurostimulator devices who have not achieved optimal benefit should consider consultation with an NSPC provider for revision surgery. Dr. Snyder successfully performs revision surgeries regularly in addition to initial implantation.
An obvious scenario for revision would be a patient presenting with broken neuromodulation device hardware that was previously beneficial.
Dr. Snyder also provides second opinions for patients who are status post neurostimulator device placement with continued pain. He can perform surgery for revision of inadequately placed neurostimulators in patients whose existing neurostimulators produce suboptimal results.
A more complex issue is whether someone with an existing implanted neuromodulator device should consider revision surgery with a different device. Technology is advancing at a tremendous pace, especially in medicine. This holds true for neuromodulation devices, which are rapidly evolving, resulting in more versatile and efficacious treatments. If an improved model has come on the market and the present device isn’t meeting the patient’s expectations, a newer device may be the appropriate choice.
“There are frequently newer models and different studies that are improving the landscape for patients with chronic pain,” Dr. Snyder says. “What’s happening in the field is very exciting.”
So, when should patients with relatively outdated neuromodulation devices consider revision surgery? If everything is functioning well and the patient’s pain is optimally controlled, revision surgery is not necessary. However, patients who have previously had a neuromodulation device placed with suboptimal pain control should be referred for a consultation to see whether a newer model or perhaps a different device would be appropriate and beneficial for them. At NSPC, these patients are evaluated on a case-by-case basis to assess the appropriateness of revision surgery.
“If you have a system inside your body and it is not helping as much as you would like — whatever the reasons — a revision may offer you a chance at further improvement,” Dr. Snyder says.

Neuromodulation Devices Available at NSPC
- Deep brain stimulation
- Dorsal root ganglion stimulation
- Intrathecal pumps
- Motor cortex stimulation
- Occipital nerve stimulation
- Peripheral nerve stimulation
- Spinal cord stimulation
- Vagal nerve stimulation
Care Following Neuromodulator Device Placement
The recovery time following neuromodulator device placement, as well as follow-up after device placement, is specific to the neuromodulator and individual patient needs. Some device placement surgeries are minimally invasive and only require a short recovery time, while others may have a longer recovery.
Patients often need relatively close follow-up in the early days following the procedure. During this time, providers make fine adjustments to the device to make sure it is working optimally and to ensure that pain is well-controlled.
“Beyond the initial calibration of the device, there is very little necessary follow-up,” Dr. Snyder says. “Most of the devices will alert the user that the battery is getting low. Certainly, if someone has pain that is worsening, they are going to come back to the doctor, and if a low battery is the cause we will step in to assess the situation very rapidly.”
While most neuromodulator devices are operated by battery power, many can last several years. Low-battery alerts and a return or increase of the original complaint are reasons to contact the surgeon who implanted the device.
“What drives me personally is the opportunity to make a difference in people’s lives. Sometimes that can be done on a very small scale, which still makes a big difference. Other times it can seem almost miraculous.”
— Brian Snyder, MD, neurosurgeon at NSPC
Toward an End to Pain
With these advancements in neuromodulation devices, patients with chronic pain have more options for pain control now than ever before. Neuromodulation is becoming more advanced and versatile, offering hope to those with chronic pain that has been refractory to treatment. Often, patients have multiple options for neuromodulation treatment modalities. Dr. Snyder welcomes the opportunity to share these advances with people who may have struggled with pain for years.
“There’s a large opportunity to make a major difference in many people’s lives,” Dr. Snyder says. “We really want to see anybody who is suffering with chronic pain, including patients who have had unsuccessful attempts at neuromodulation or suboptimal implants.”
Learn more about neuromodulation devices offered at NSPC Brain & Spine Surgery by visiting nspc.com.
Source: MD News March 2022, Long Island Edition
