Growing research into COVID-19 supports that underlying conditions such as hypertension, Type 2 diabetes and obesity, factor into the severity of patient disease and health outcomes, including heightened mortality rate. Dr. Atwa and his colleagues at Long Island Laparoscopic Doctors are helping shape the future of treating obesity and its associated conditions in the face of a global pandemic.

As the world awaits the development of a proven vaccine and therapeutic treatments for the new coronavirus, clinicians and researchers have prioritized identifying which patients are most likely to suffer the gravest impact of the disease and potentially need the most medical resources to survive. Data show that patients older than 65 and those with preexisting health conditions develop more severe, and often deadly, symptoms. These conditions have a common thread — obesity.
An Increasingly Vital Option for Better Health
Bariatric surgery has been called “medicine’s best and most underused tool” to combat obesity, and Long Island Laparoscopic Doctors is a regional leader in bariatric surgery.
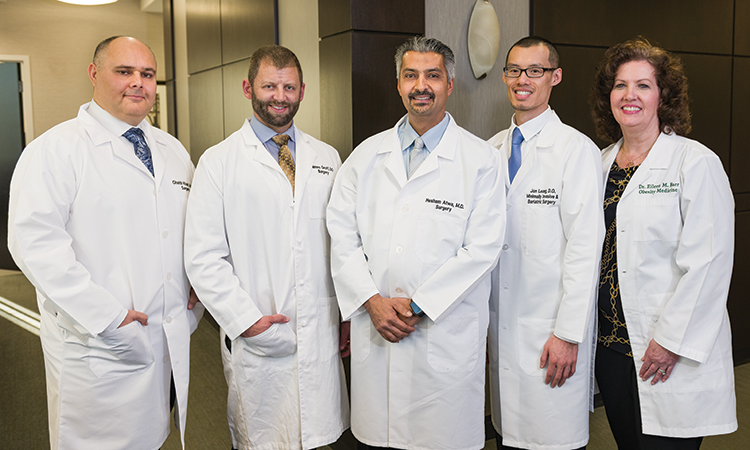
Hesham Atwa, MD, FACS, FASMBS, is the Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors in East Setauket. Dr. Atwa and his team of experienced bariatric surgeons, which includes Jon Leung, DO, and Ghaith Khair, MD, have performed hundreds of bariatric procedures at Long Island Laparoscopic Doctors. In doing so, they added years to each patient’s life while reversing health conditions such as Type 2 diabetes, heart disease, sleep apnea and joint pain, which are most often associated with obesity.

Dr. Atwa says using advanced robotics on patients who are severely obese allows Long Island Laparoscopic Doctors’ to take a less invasive approach to bariatric surgery, resulting in shorter hospital stays and less risk overall for patients. These benefits are due to innovations and advancements made possible by the most advanced surgical technology available — the da Vinci Xi surgical robotic system.
Addressing Bariatric Surgery With Patients
“Obesity affects more than 40% of the U.S. population, and bariatric surgery is the best tool we have to treat it,” Dr. Atwa says. “Approximately 25 million people qualify for bariatric surgery, but surgeons only perform about 225,000 cases each year.”
Studies show that most patients who elect to have bariatric surgery maintain long-term weight loss, which is far more successful than diets, exercise and other lifestyle modifications. However, the challenge of convincing patients to take this step is significant for healthcare professionals. Prospective patients tend to underestimate their obesity, and relatively few eligible adults choose weight-loss surgery as a solution. To educate people about the power of bariatric surgery and its benefits, medical providers need to address the barriers that prevent patients from seeking surgery. The two most common barriers include providers failing to reinforce surgery as a weight-loss option, and patients assuming the cost of the surgery is high.
Fewer than 1% of eligible bariatric surgery patients receive the surgery each year.
According to the CDC, people of any age are at higher risk of developing severe illness from COVID‑19 if they have a BMI of 30 or higher.
The rate of obesity has almost tripled worldwide since 1975.
Despite growing recognition that weight-loss surgery can be beneficial, bariatric surgery occupies less of a presence in consumers’ minds than dieting, exercise or weight-loss supplements. Surveys show that of individuals who meet the criteria for bariatric surgery and have recently interacted with the healthcare system, only 12% were told they were eligible for surgery by a doctor. Issues such as time with patients and uncertainty about patients’ eligibility may prevent primary care providers and others from discussing bariatric surgery with their patients. However, the recent COVID-19 crisis makes it especially important for providers to hold at least a brief conversation with a patient at risk who could have a longer and healthier life after bariatric surgery.
Of patients who have considered bariatric surgery but do not follow through, 40% said the main reason was cost. Most bariatric practices can help a patient qualify with their insurance company, and if they don’t have available health coverage, financial payment plans are available. A severely obese patient with comorbidities, such as Type 2 diabetes or high blood pressure, should take into account the full range of healthcare expenses, including care related to the consequences of poor health, as well as missed days of work, when estimating the actual financial cost of their decision.
“We in the United States have not always identified obesity as a disease, and some people think it is a lifestyle choice, but it’s not. It makes people sick, and obesity must be seen for what it is, a pandemic by the same definition as the coronavirus.”
— Hesham Atwa, MD, FACS, FASMBS, Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors
Bariatric Surgery During the Pandemic
Dr. Atwa believes important lessons are to be gained from the nation’s experience with COVID-19. Treating obese patients with significant comorbidities within the scope of a pandemic requires greater synergy between primary care physicians and other specialists, such as cardiologists, endocrinologists, bariatric surgeons and bariatricians. Furthermore, he believes the fight against obesity requires support from the government and insurance companies, as well as full and affordable health insurance. Above all, reducing rates of obesity requires patient education.
The Obesity and COVID-19 Connection
 The World Obesity Federation issued a statement concerning obesity and COVID-19 indicating that obesity-related conditions seem to worsen the effects of COVID-19. According to The Obesity Society, the severity of the disease intensifies in people with respiratory conditions and those with compromised immune systems. Because people with obesity often have these comorbidities, they are considered at higher risk for developing a severe form of the disease.
The World Obesity Federation issued a statement concerning obesity and COVID-19 indicating that obesity-related conditions seem to worsen the effects of COVID-19. According to The Obesity Society, the severity of the disease intensifies in people with respiratory conditions and those with compromised immune systems. Because people with obesity often have these comorbidities, they are considered at higher risk for developing a severe form of the disease.
The Centers for Disease Control and Prevention (CDC) reports that people of any age with certain underlying conditions are at increased risk for developing a more severe form of COVID-19. These conditions include heart disease, Type 2 diabetes and obesity. According to data from the CDC, the obesity rate in the U.S. reached 42.4% in 2017–2018, and data from COVID-NET reveals that nearly 90% of hospitalized patients had one or more underlying health conditions. The most common of these were obesity, high blood pressure, diabetes, lung disease and heart disease.

Two studies that analyzed data from approximately 4,000 patients who sought care for COVID-19 at NYU Langone Health in March and April revealed that obesity — more than diabetes and high blood pressure — was shown to be a greater risk factor for hospitalization and death. The study listed obesity as the most significant risk factor, after older age, for being hospitalized with COVID-19. While the findings are preliminary, the study suggests that for those under age 60, obesity is the top underlying factor providers should focus on in these patients.
Patient Eligibility for Weight-Loss Surgery
Typically, individuals qualify for bariatric surgery if they have a body mass index (BMI) of 40 or higher or a BMI of 35 or higher and at least one comorbidity. Dr. Atwa and his colleagues at Long Island Laparoscopic Doctors offer a variety of bariatric surgery options, including gastric bypass and gastric sleeve — and revision procedures for both — as well as conversion from gastric band to gastric sleeve. Endoscopic insertion of the Orbera gastric balloon is available for patients who do not qualify for bariatric surgery or prefer a nonsurgical option. Medical weight loss is also available as a stand-alone treatment, as a complement to the Orbera gastric balloon or to help patients lose weight while they prepare for robotic-assisted surgery.
Poised to Help More Patients
A key factor transforming bariatric surgery and increasing its appeal to patients and providers is robotic-assisted surgery, and Dr. Atwa and Long Island Laparoscopic Doctors are on the leading edge of this shift. Dr. Atwa uses the da Vinci Xi surgical system to perform gastric bypass and gastric sleeve procedures at St. Charles, Mather and St. Catherine hospitals, which are part of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program – Centers of Excellence for Bariatric Surgery.
“Performing a robotic-assisted bariatric procedure is less taxing for the surgeon, which results in fewer complications, especially with revision procedures that involve a lot of scar tissue. The 3D visualization helps create a more accurate procedure,” Dr. Atwa says. “Performing a laparoscopic operation on an obese patient involves a lot of positioning, but with da Vinci, the surgery is the same whether I am operating on a 200-pound patient or a 500-pound patient.”
Partnering With Referring Providers
A variety of barriers prevents primary care providers and other physicians from discussing bariatric surgery with patients and referring them to learn more about it. Those barriers include time constraints, uncertainty about patients’ eligibility or whether insurance providers will cover the procedure, and lack of awareness about bariatric surgery as a treatment option for obesity. Long Island Laparoscopic Doctors seeks to help referring providers and patients alike learn more about bariatric surgery with education in a variety of media, including a brochure, a website (journeytothenewyou.com) and an app (Baritastic — practice code 066333). Having support from referring physicians is crucial to patients’ success.
“Referring physicians help us get patients in the best shape possible before surgery,” says Hesham Atwa, MD, FACS, FASMBS, Director and Chief of Surgery at St. Charles Hospital, Chief of Surgery at Mather Hospital Northwell Health, and Founder and Clinical Director of Long Island Laparoscopic Doctors. “After surgery, we depend on them to adjust patients’ medications as conditions, such as hypertension, improve.”
For more information, visit journeytothenewyou.com.
